When one mental health problem starts, it often triggers other mental health problems to start as well. How can we understand this better, and how can we tackle it better?

When we hear the term “mental illness”, the first thought that crosses our mind is usually depression or anxiety. The truth is, there are 5 editions of the Diagnostic and Statistical Manual of Mental Disorders (DSM), 947 pages and more than 250 classified mental disorders with multiple subtypes of each. The disability-adjusted life year (DALY) is a measure of overall disease burden, expressed as the number of years lost due to ill-health, disability or early death. In other terms, it is how many years a person loses when they become a dysfunctional member of a society due to an illness, be it physical or mental – i.e. they skip school, work or simply do not pursue their goals. Thirty years ago, infections and diarrhea were the leading causes of global burden of disease. Recently, depression and anxiety disorders have worked their way up the ladder and are expected to become the 2nd leading cause of burden of disease in 2020 (WHO).
A tremendous amount of effort has been directed towards eliminating social stigma towards mental disorders. However, little has been done to improve the concept of self-stigma whereby a person stigmatizes against themselves for having a mental illness. Statements like, “I am weak and unable to care for myself!” often lead to negative emotional reactions, especially low self-esteem, and self-efficacy. Because of this self-prejudice, persons with mental disorders may fail to pursue appropriate work opportunities or achieve their goals. This is not only due to their mental illnesses but rather a combination of both, the illness as well as their self-prejudice which hampers their functionality as individuals and prevents them from seeking medical help.
An approach to mental illness is to think of it as a cycle. For instance, a person with a binge eating disorder may also suffer from Body Dysmorphic Disorder (BDD) which is defined as the preoccupation with at least one nonexistent or slight defect in physical appearance (DSM V, 2013). These concerns about appearance lead to repetitive behaviors (eg, mirror checking, excessive grooming, or skin picking) or mental acts (eg, comparing one’s appearance to that of others). The result could be in the form of significant distress, psychosocial impairment, dissatisfaction, and continuous efforts to change body image which may eventually lead to depression. To deal with depression, the person might further engage in binge eating which causes nothing but a vicious cycle of binge eating, body dysmorphic disorder, depression, and anxiety. To break this vicious cycle, we need to target the individual components that make it up: the disorders and the self-prejudice associated with them.
Unfortunately, mental illnesses are often co-morbid – i.e. they exist simultaneously. The issue of under-diagnosis due to patients not seeking medical help makes matters worse, as most mental illnesses are left untreated. Currently, 1 in 5 people suffer from depression. Another 1 in 50 people around the world are preoccupied with their skinny bodies, oversized hips or a bump on their nose. These numbers are merely the tip of the iceberg which signifies the grave importance of diagnosing these illnesses and treating them as soon as possible.
With the continuous change in the patterns of body perception that we see with each decade, it is no doubt that at every point in time, someone is dissatisfied with how they look. For instance, men who suffer from muscle dysmorphic disorder – a subtype of BDD – constantly compare their bodies to other men which lead to depression, anxiety, and dissatisfaction. In the early 1900’s, people tried to eat as much as possible to get the “Fat” look – a sign of wealth and higher social status. Fast-forward 100 years, people are now going under the knife to carve their bodies to their satisfaction or following extreme diets and workout routines to become lean and bulky.
As such, it is important to recognize the patterns and cycles of mental disorders that we see in our societies and the causes that led to their evolution. Instead of comparing our bodies to the “ideal” for our time, a better approach would be to pursue a healthy lifestyle, achieve a medically fit body and practice a sport we actually like. Weightlifting, for example, has become a widespread and trendy sport. So much so, that even people who don’t like weightlifting try to pursue it in order to achieve the millennial lean and bulky look. Yet, unfortunately, they end up quitting too soon.
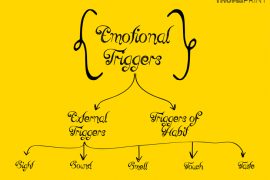
Treatment options for BDD and its other co-morbid illnesses involve the use of drugs – pharmacotherapy– and cognitive-behavioral therapy (CBT). CBT for BDD must be tailored to specifically address BDD’s unique symptoms; otherwise, it is unlikely to be helpful. This necessitates consulting a medical professional which is often neglected, especially in our part of the world. Techniques used in CBT include, but are not limited to, psychoeducation, goal-setting, eliminating exposure to triggers, prevention of rituals, and habit reversal. The introductory sessions are often motivational after which advanced cognitive strategies target the core elements of BDD such as excessive mirror checking, core beliefs (e.g., “I am worthless”), and relapse prevention. Not to mention pharmacological intervention which is also required based on the severity of the illness and can be addressed by a mental health professional only.
To tackle these issues, we should start by engaging in sports we actually enjoy for their mere health benefits, seeking medical help for any signs of mental disorders, increasing efforts to eliminate self-prejudice, and increasing motivation and self-acceptance. Only then will we be taking the first step in breaking one of the most common cycles of mental health disorders among youth today: body image disorders, eating disorders, and depression.
References:
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), American Psychiatric Association, Arlington 2013.
- 2017. Body dysmorphic disorder: Treatment and prognosis. [ONLINE] Available at: LINK. [Accessed 1 April 2018].